Here’s my reaction from yesterday. I’m assuming you already read Dave’s write-up. Hopefully, by getting it all down and out of my head, I’ll be able to relax a bit more. I don’t think I took yesterday as hard as Dave because I did my grieving after the first visit, but my waking up at 5:30 this morning says that I’m still deeply affected.
Yesterday was long. Over 5 hours of appointments, we talked to 9 different people: a NICU neonatologist, a social worker, a sonographer, a pediatric cardiologist, a perinatal physician, a research study representative, another social worker, a pediatric cardiac surgeon, and a cardiovascular child life specialist. Additionally, we toured both the NICU and the Cardiovascular Care Center (CVCC, the cardiac specific ICU at Children’s) .
Yesterday was a mixed bag. On one hand, it feels good to have a definite plan. On the other hand, medically it felt like we took two steps back, and the plan is pretty crappy. I’d use a different word, but with a kid coming, I need to cut back on my swearing.
The Bad
The echo was consistent with the previous times, with no relative improvement. She is still borderline HLHS. They still won’t be able to decide what surgery she needs until after she is born. It was decided that our daughter’s heart is so bad that we are skipping the NICU, and going straight to the CVCC. One drawback to that is the CVCC is not as used to babies. That makes it less likely that we will be able to hold her while she is there. Additionally, there are no webcams at the CVCC like at the NICU. That will make it harder for Dave to feel connected when he has to work. Of course, we are already working on a plan to provide our own webcam using our baby monitor.
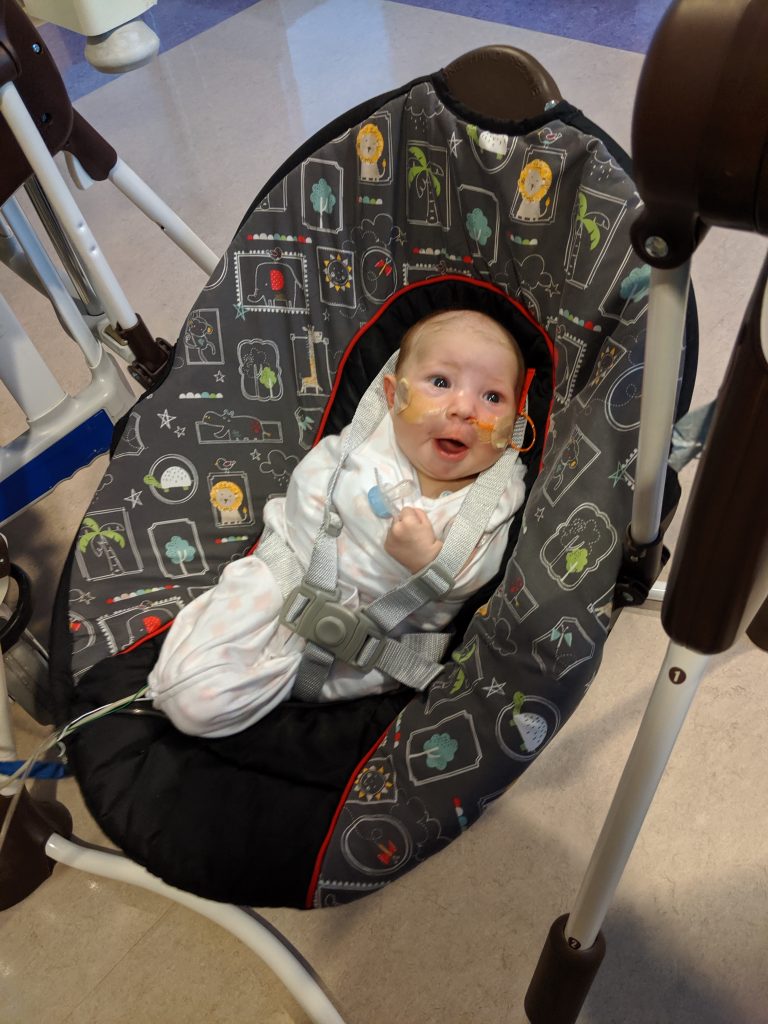
It was also decided that PGE needs to be started in the first hour. That means she has to be immediately hooked up to all the bells and whistles of a hospital. The after birth time will be nothing like normal, and has the potential for great sadness. At least the cardiologist took the time to explain exactly why we are doing this, and I have to agree with the decision.
Another implication of her unknown heart status at birth is that she will not be receiving any nourishment by mouth for the first bit. Since they don’t know how effective her blood flow will be, they don’t want to divert any away from important things like the brain to go to the gut for digestion. She will get all her nutrients from an IV. Once she does start eating, it will be a slow ramp up that takes at least a week. I guess I’ll become well acquainted with pumping.
I was also sad that the set of 3 surgeries to replumb an HLHS heart were so strongly back on the table. I was so hoping that it would just be a simple aortic repair. It still might be, but it is not as hopeful as after echo #2. At least the surgeon took the time to explain exactly how they will be deciding if our daughter ends up with 1 or 2 ventricles. I am happy that it is extremely data driven, with a few separate statistical models for decision making in the 3 separate calculators they will use.
If we do have the set of 3 surgeries, our summer will be very different than we had hoped and planned. Yes, we were leaving 2 months unplanned, but we had started putting trips on the calendar for when she was 3 months old and beyond. Now, we might not be able to do those trips. Even my brother’s wedding in September in Boston has the strong likelihood of being impacted.
No matter what, she needs surgery before she comes home, at least to expand the aorta. That surgery can’t happen until she’s almost a week old. That puts minimum time at the hospital to over 2.5 weeks. A month is more likely, and 2 months is not unheard of.
We still don’t have buy in from the hospital staff about our ideal birth scenario. Talking with the NICU staff made me realize that we need strong buy in to keep anything resembling normalcy in our birth experience. I wrote a long email, and am waiting for a response. At least I’ve been warned. NICU people are very intense.
Another crappy thing is that we are still fighting billing for our first visit in December. I hate how, just because Allina and UCare are having a pissing contest, we pay the literal price in terms of thousands of dollars.
The Good
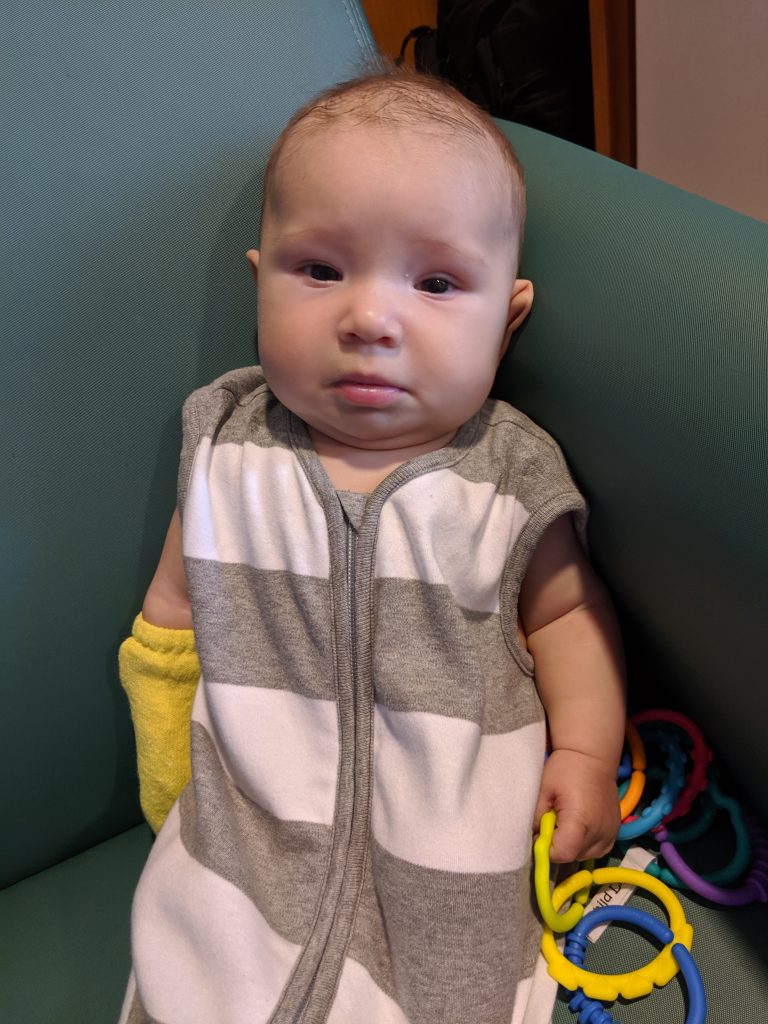
With the two tours, we have a good idea of what to expect for the time we are at the hospital. For a hospital, they try really hard to make it a pleasant experience with lots of resources, like a parents’ area in every room, room fridges, the Ronald McDonald house, kid friendly accessories, etc.
The Mayo Clinic is running a research study for HLHS babies that involves cord blood. Dave and I had it on our list to look into it. Instead, a study rep came to us and invited us to join the study. They are just entering phase 2, which means phase 1 showed safety and improvement. The surgeon was even excited about it.
Even though the aorta has crappy flow, the heart has good function. It is unknown if the left ventricle has adequate function, but it looks good. After birth, they will do two different echos, one immediately in the first hours, and then another at around 3 days. There, they can measure the specifics like left ventricle ejection fraction, etc. Those numbers will be fed into the calculators to decide if the left ventricle is adequate. It won’t just be one doctor’s gut decision.
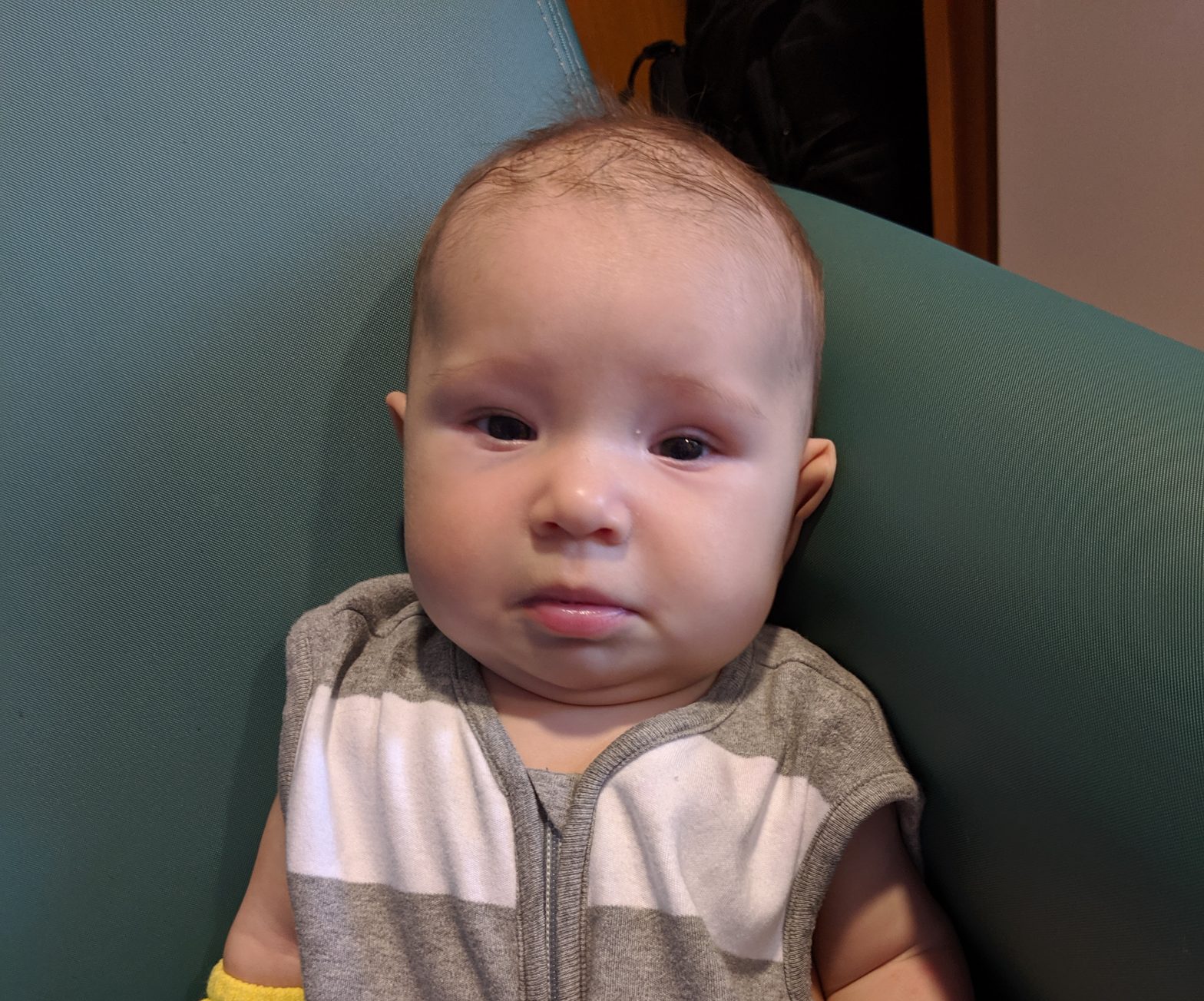
She is still growing normally. She is at the 67th percentile, with an estimated weight of 4lbs 9oz. Of course with Dave’s big head, her head hit the 90th percentile. It was cute to see hair on the ultrasound. It might even have a bit of a curl.
We are happy with our decision to be at Children’s Minnesota. They handle more cases like this than both Mayo Clinic and the University of Minnesota combined. They do less than Boston, but the advantages of a local hospital win out.
I am relieved that they are okay with us staying with the midwives from the Minnesota Birth Center. The normal procedure for congenital heart defects is to have labor induced. I don’t want that. With the midwives, that is way less likely, and I am pretty confident they will only induce if medically necessary. Additionally, the chances of an uncomplicated natural vaginal birth are much higher with the midwives. That will make it more likely that I can go with our daughter to the CVCC, and we won’t be immediately split up.
I think that is it. They decided that will be our last echo before birth. Hopefully, I won’t see any of those people until after a peaceful, natural birth in April. Now, let’s see if I can actually get some sleep.