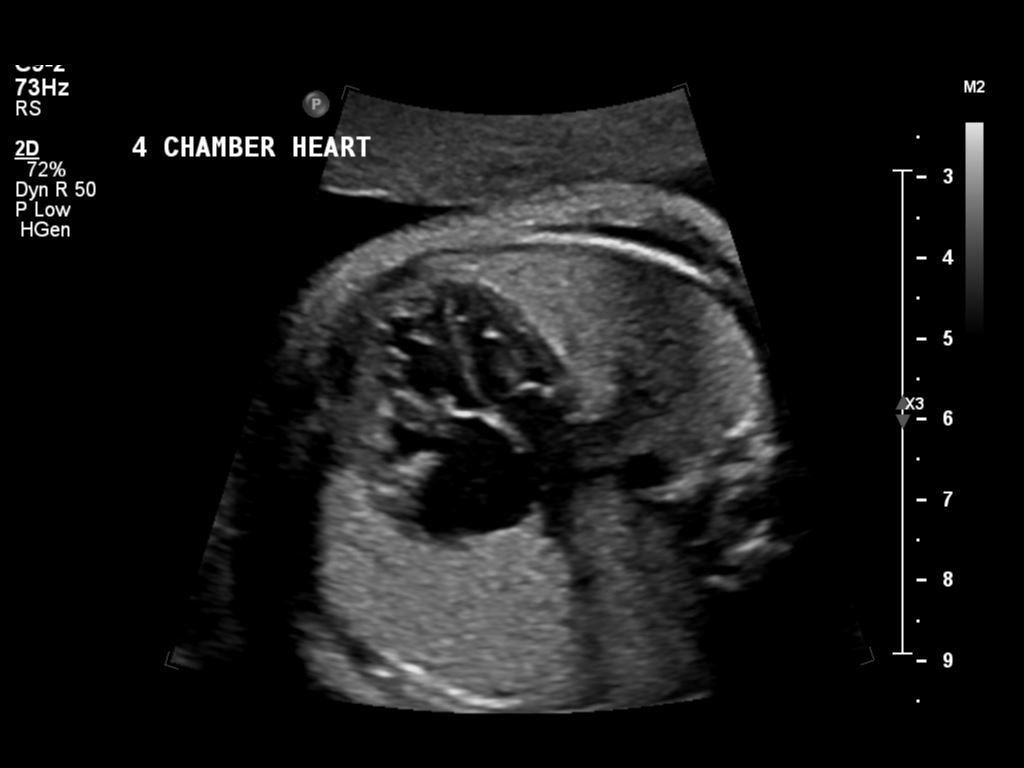
Today we had ultrasound number three with the Perinatal Physicians. Audrey is at 32 weeks tomorrow. We got a 3rd chance to see how our little one’s growth has progressed and talk in detail for the plans for birth.
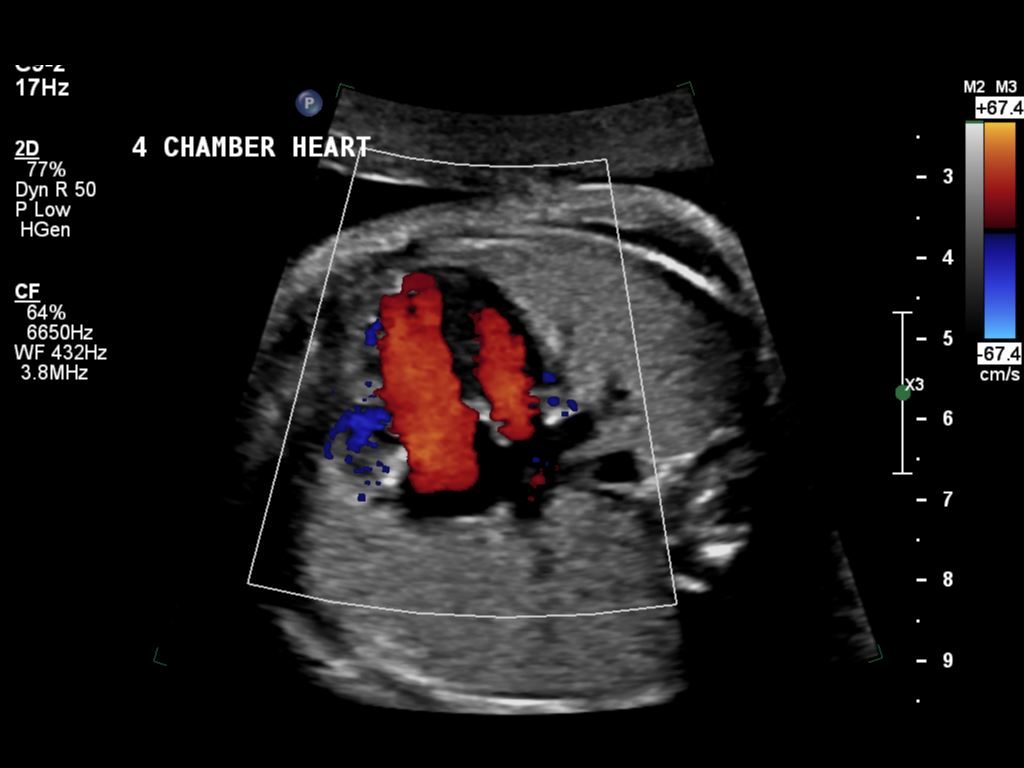
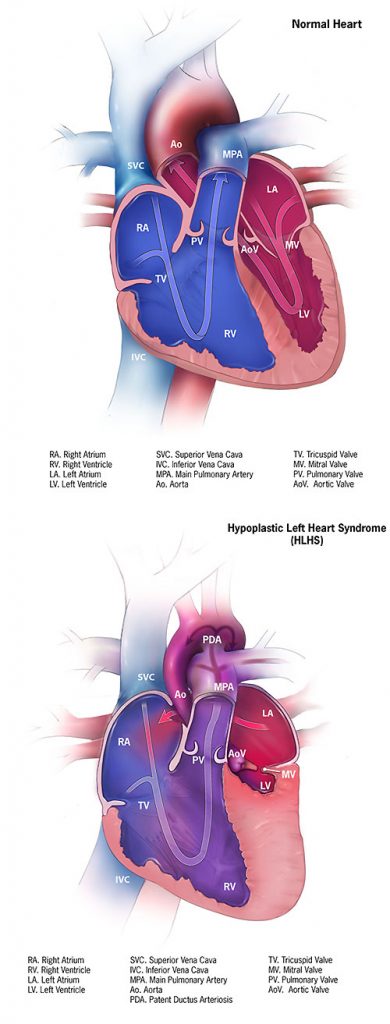
The short version is, not much change. Our daughter will be in the Cardiac Intensive Care Unit within 30-60 minutes of being born. We were hoping for a little more bonding time before that happened but everyone believes it is critical to get on PGE (the drug that stops the ductus in the heart from closing) as soon as possible. They will also be doing the heart echo and other tests then determining what is needed. It’s all but certain that some kind of heart surgery will be needed within the first 1-2 weeks. If she has full-blown HLHS, it will be the scary first of three surgeries to re-plumb her heart into a 2-chamber vessel. The better outcome will be she only needs a surgery to widen her aorta.
It was an emotional day. It’s getting more and more real that we’re having a baby and the realization of what the heart issues mean is growing. There’s going to be ventilators and monitors and IVs and no telling how much, if any, holding of her we’ll be able to do.
It’s scary not knowing what will happen. If she has full-fledged HLHS, it’s a very tough and challenging process. The period in between the first surgery, immediately after birth, and the 2nd surgery, around 4-6 months, is a fragile period where we have to watch out for illness and monitor things very carefully. It’s amazing to think that we are hoping she’ll only need an aortic graft!
This was the last big ultrasound with the fetal echo before birth, unless something else comes up. At birth, there will be a team from the neonatal intensive care unit to do the immediate assessment. Hopefully we’ll get a little time with her before they whisk her away to get started on her journey.
I am finding this tough. I’m a fixer. I want to do something to help fix the problem and all I can do right now is prep and be supportive to Audrey. At birth, I’m going to initially have to split my time between Audrey and the baby as the little one will likely be at Children’s before Audrey is stable and able to make it over to us. Big breath. Lots of emotions.
Even with the above, I am still extremely happy we have resources like Children’s Hospital so close by! It was helpful to meet all the staff, from the cardiologist to the surgeon, the perinatologist, care coordinators and social worker.
Thanks to all the friends and family who are helping us in this process. We appreciate the support and we’re going to keep needing it.